Patents on key biological medicines used in rheumatology will expire soon. The European Medicines Agency’s (EMA’s) finalized guidelines on biosimilar monoclonal antibodies (mAbs) came into effect on 1 December 2012. Both of these facts mean that rheumatologists can expect to be exposed to biosimilars of the medicines they routinely use in the near future.
Biosimilars in rheumatology
Biosimilars/Research
|
Posted 29/03/2013
 0
Post your comment
0
Post your comment

But what can they expect? When it comes to biosimilars there is often much talk of the complexity of the molecules, the chances for microheterogeneity and the fact that they are not identical, but only similar to the reference biological. Small changes in their manufacturing process, such as pH, temperature and culture media ingredients; can affect the final product. This has lead to ‘concerns’ about their use, however, these facts are not exclusive to biosimilars; they apply to originator biologicals as well.
Author Dr Christian Schneider highlights the similarities of EMA approval process for originator biologicals and biosimilars, thus demonstrating the fact that biosimilars are of the same high quality, and are as safe and effective as originator biologicals [1].
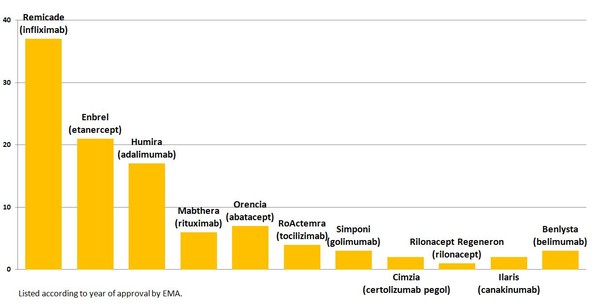
Changes in the manufacturing process for originator biologicals used in rheumatology follow the same scientific principles as that used to approve a biosimilar. And, in fact, all of the licensed mAbs and -cept fusion proteins used in rheumatology have had changes in their manufacturing processes after their initial approval, see Figure 1.
Figure 1: Changes in the manufacturing process for EMA approved biologicals used in rheumatology
The EMA regulatory review procedure uses dedicated experts in analytical, physicochemical and biological characterization to prepare an assessment report. The Committee for Medicinal Products for Human Use (CHMP) Biologics Working Party (BWP) then adopts a list of questions for the applicant based on review of this report. The median number of questions asked for currently authorized biosimilars was 119, compared with 121 for authorized mAbs/cepts used in rheumatology. This shows that the regulatory review process for biosimilars is as critical as for originator biologicals.
Schneider makes it clear that the same microheterogeneity often mentioned with respect to biosimilars is also found in batch-to-batch variability of reference biologicals.
Scheider argues that biosimilars do not in fact undergo an accelerated or abridged approval, as the time from the start of the regulatory review process to a positive outcome being issued by CHMP was not shorter for the biosimilars authorized to date compared with originator mAbs/cepts used in rheumatology.
Conflict of interest
The author of the research article declared that there was no conflict of interest.
Related articles
Development of biosimilars for rheumatology
Challenges in the development of biosimilars mAbs
Reference
1. Schneider CK. Biosimilars in rheumatology: the wind of change. Ann Rheum Dis. 2013;72(3):315‑8.
Permission granted to reproduce for personal and educational use only. All other reproduction, copy or reprinting of all or part of any ‘Content’ found on this website is strictly prohibited without the prior consent of the publisher. Contact the publisher to obtain permission before redistributing.
Photo credit: rcpi.ie
News
EMA recommends approval for teriparatide biosimilar Zandoriah
FDA approves third interchangeable ranibizumab biosimilar Nufymco
General
Samsung Bioepis wins Pyzchiva case; Regeneron patent rulings threaten foreign biosimilars
Chinese biosimilars go global: growth, partnerships, and challenges
What is the future for the US biosimilar interchangeability designation

Biosimilars/Research Posted 05/06/2025
Biosimilar clinical efficacy studies: are they still necessary?

Biosimilars/Research Posted 27/05/2025
The best selling biotechnology drugs of 2008: the next biosimilars targets








Post your comment