Biosimilars/Research
Switching to biosimilar infliximab in IBD patients
Biological agents, such as infliximab, have transformed the outcomes of patients with immune-mediated inflammatory diseases. The advent of biosimilar treatment options, such as CT‑P13 (Remsima/Inflectra), promises to improve the availability of biological therapy.
Biosimilars in oncology in the US
As part of the Affordable Care Act of 2010, the Biologics Price Competition and Innovation Act of 2009 (BPCI Act) allows for an abbreviated license pathway for the approval of biosimilars in the US. In light of continuing increases in healthcare costs, particularly for cancer drugs, use of biosimilars is increasingly being considered as a strategy for containing the cost of cancer care, according to Dr Gary Lyman of the Fred Hutchinson Cancer Research Center and University of Washington, Seattle, WA, USA [1, 2].
Loss of efficacy after switching to biosimilar infliximab in Behcet’s patients
Authors from the Division of Rheumatology at the Hospital of Prato, Italy report on three patients with Behçet’s disease that experienced disease relapses after switching from the originator infliximab, Remicade, to biosimilar infliximab [1].
Opportunities and challenges for biosimilars in oncology
The rapid increase in healthcare costs, particularly for cancer drugs, has had a major impact on providers, practices, payers and patients, according to Dr Gary Lyman of the Fred Hutchinson Cancer Research Center and University of Washington, Seattle, WA, USA [1, 2].
Phase III switching data support long-term efficacy and safety of rituximab biosimilar Truxima
Results of a phase III extension study have shown that Celltrion Healthcare’s (Celltrion) rituximab biosimilar (Truxima, CT-P10) is comparable to Roche’s MabThera/Rituxan, according to the South Korean biotechnology company.
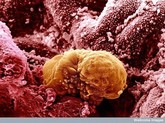
Physicochemical and biological characterization study of copy biological tocilizumab
Researchers in China have developed a copy biological of F. Hoffmann-La Roche’s (Roche) arthritis treatment Actemra (tocilizumab). A recent study compares it to the originator, finding it to be highly similar in terms of its physical, chemical and biological characteristics [1].
Australian prescribers’ views on biologicals naming and substitution
In a survey of 160 prescribers of biologicals in Australia, over three quarters agreed that the country’s Therapeutic Goods Administration (TGA) should insist on distinct non-proprietary scientific names for all biosimilars and reference products. The results of the survey were published just as TGA launched a public consultation on proposals for potential biological naming systems. A clear majority (98%) of prescribers who took part in the survey, run by the Alliance for Safe Biologic Medicines (ASBM), said they currently used either brand name or non-proprietary scientific names for recording and prescribing biosimilars and reference products [1]. Most (61%) wanted TGA to play a major role in naming biosimilars.
Biosimilar insulins – reducing the cost of diabetes
Will biosimilar insulins be cheaper is a question raised by authors Lutz Heinemann and Alan Carter and one that they say is a clear yes [1].
European perspective on biosimilars
In the European Union (EU), a legal framework for approving biosimilars was established in 2003. The first biosimilar Omnitrope (somatropin) was approved in 2006 [1].
Anti-drug antibody assays for biosimilars and originator biologicals
Biosimilar drug development has brought new challenges to bioanalytical ligand-binding assays used to determine drug concentration, anti-drug antibodies and neutralizing antibodies.