New therapies are needed to manage the increasing incidence, severity, and high rate of recurrence of Clostridium difficile infection in which toxins A and B cause pseudomembranous colitis. This is associated with bleeding and a severe form of diarrhoea, which together can lead to perforation of the lower bowel and even death.
Medarex: With CDA1, CDB1 MAbs better metronidazole or vancomycin treatment against C difficile toxins
Biosimilars/News
|
Posted 16/02/2010
 0
Post your comment
0
Post your comment

Israel Lowy and Deborah Molrine et al. of MassBiologics, University of Massachussetts Medical School at Boston, MA, USA, performed a clinical trial on two monoclonal antibodies (MAbs) against Clostridium difficile infection (licensed by Merck & Co. in April 2009), which was sponsored by Medarex in Princeton, NJ, USA (recently acquired by Bristol-Myers Squibb). The outcomes of this study have been published in the New England Journal of Medicine issue of 21 January 2010.
Drs Lowy and Molrine performed a randomised, double-blind, placebo-controlled study of two neutralising, fully human MAbs against the C difficile glucosyltransferases toxin A (MDX-066 or CDA1) and toxin B (MDX-1388 or CDB1). The antibodies were administered together as a single infusion, each at a dose of 10 mg per kilogram of body weight, in patients with symptomatic C difficile infection who were receiving either metronidazole or vancomycin as antibiotic agent. The primary outcome was laboratory-documented recurrence of infection during the 84 days after the administration of MAbs or placebo. They found that among the 200 patients who were enrolled (101 in the antibody group and 99 in the placebo group), the rate of recurrence of C difficile infection was lower among patients treated with MAbs (7% vs. 25%; 95% confidence interval, 7 to 29; p < 0.001). The recurrence rates among patients with the epidemic BI/NAP1/027 strain were 8% for the antibody group and 32% for the placebo group (p = 0.06); among patients with more than one previous episode of C difficile infection, recurrence rates were 7% and 38%, respectively (p = 0.006). The mean duration of the initial hospitalisation for inpatients did not differ significantly between the antibody and placebo groups (9.5 and 9.4 days, respectively). At least one serious adverse event was reported by 18 patients in the antibody group and by 28 patients in the placebo group (p = 0.09).
The authors concluded that the addition of CDA1 and CDB1 MAbs against C difficile toxins to the antibiotic agents metronidazole or vancomycin significantly reduced the recurrence of C difficile infection. These MAbs may therefore be interesting biosimilar targets.
References:
Israel Lowy and Deborah Molrine et al. Treatment with Monoclonal Antibodies against Clostridium difficile Toxins. NEJM 362:3;197-205. 2010 January 21.
Study of the Clinical Effectiveness of a Human Monoclonal Antibody to C. Difficile Toxin A and Toxin B in Patients With Clostridium Difficile Associated Disease.
Pharmas are making smaller deals - Small biotech has the goods. Nature. October 2009.
Source: NEJM; Nature
Research
Reaching ESG goals in pharmaceutical development
What is the future for the US biosimilar interchangeability designation
General
Samsung Bioepis wins Pyzchiva case; Regeneron patent rulings threaten foreign biosimilars
Chinese biosimilars go global: growth, partnerships, and challenges
Most viewed articles
The best selling biotechnology drugs of 2008: the next biosimilars targets
Global biosimilars guideline development – EGA’s perspective
Related content
FDA approves Poherdy (first interchangeable pertuzumab) and Armlupeg (pegfilgrastim) biosimilars
EMA recommends approval for insulin glargine biosimilar Ondibta and denosumab biosimilar Osqay
FDA approves denosumab biosimilars Osvyrti and Jubereq, Boncresa and Oziltus
FDA approves aflibercept biosimilar Eydenzelt and label expansion for adalimumab biosimilar Yuflyma
FDA approves Poherdy (first interchangeable pertuzumab) and Armlupeg (pegfilgrastim) biosimilars
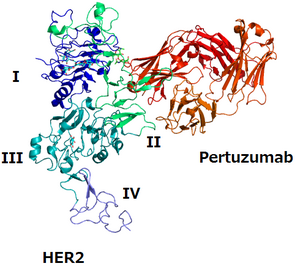
Biosimilars/News Posted 27/01/2026
EMA recommends approval for insulin glargine biosimilar Ondibta and denosumab biosimilar Osqay

Biosimilars/News Posted 16/01/2026
FDA approves denosumab biosimilars Osvyrti and Jubereq, Boncresa and Oziltus
Biosimilars/News Posted 07/01/2026
FDA approves aflibercept biosimilar Eydenzelt and label expansion for adalimumab biosimilar Yuflyma

Biosimilars/News Posted 05/12/2025
The best selling biotechnology drugs of 2008: the next biosimilars targets






Post your comment