As drug manufacturers await guidance on a biosimilar approval pathway in the US, the debate goes on as to how high the bar will be set for the FDA to designate a biosimilar as interchangeable. In one critical area of the law that outlines biosimilar regulations, Congress outlines the difference between biosimilarity and interchangeability with respect to biosimilars and innovative biologicals, but the FDA has yet to define the difference.
Interchangeability of biosimilars in the US
Biosimilars/News
|
Posted 27/05/2011
 0
Post your comment
0
Post your comment

Healthcare reform in the US was brought in to force in March 2010. This reform also allows for a pathway for marketing approval of biosimilar medicines, by including The Biologics Price Competition and Innovation (BPCI) Act of 2009, which established an abbreviated Biologic License Application (aBLA) pathway for the approval of biosimilars.
The BPCI Act also gives FDA the authority to designate a biosimilar as interchangeable with its reference product. This means that the biosimilar may be substituted for the originator product by the pharmacist without reference to the prescribing physician.
This is somewhat different to the situation in the EU, where the EMA does not have the authority to designate biosimilars as being interchangeable with the reference product.
Both innovator companies and patient advocacy groups in the US have objected to this automatic interchangeability, stating patient safety as the reason. Their argument is that little is known about biologicals and any impurities or minor structural or formulation changes could have unanticipated effects for patients. Some groups have suggested substantial clinical testing for biosimilars and a delay in any interchangeability determination until after post-marketing studies have been conducted on the biosimilar in question.
On the other hand biosimilar manufacturers argue that FDA is already equipped to make both biosimilarity and interchangeability determinations. There is also evidence from Sandoz, Novartis’s generics division, that quality changes in originator biologicals have been accepted by the health authorities [1].
Since the US Congress is also intent on making low-cost biosimilars available to patients it probably intended something less than full clinical trials for approval of biosimilars. Taking into account patient safety, it is therefore believed that the FDA rules will likely to be less stringent than a Biological License Application, but more stringent than is hoped by biosimilar manufacturers.
Editor’s Comment
The question is how high will the bar be set for biosimilars? Of course patient safety is paramount, but the requirements should not be set so high as to discourage competition, which will drive down prices and increase patient access to affordable medicines.
Please feel free to share your thoughts via email to editorial@gabionline.net or in the comments section below. What are your views on the progress of the biosimilars pathway in the US? What do you think the requirements will be for biosimilars to be approved and designated as interchangeable in the US?
Related articles
Interchangeability or substitution of biosimilars
Acceptable changes in quality for glycosylated biologicals
Reference
1. Schiestl M, Stangler T, Torella C, Cepeljnik T, Toll H, Grau R. Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nat Biotechnol. 2011;29(4):310-2.
Source: Patent Law Practice Center
Research
Reaching ESG goals in pharmaceutical development
What is the future for the US biosimilar interchangeability designation
General
Samsung Bioepis wins Pyzchiva case; Regeneron patent rulings threaten foreign biosimilars
Chinese biosimilars go global: growth, partnerships, and challenges
Most viewed articles
The best selling biotechnology drugs of 2008: the next biosimilars targets
Global biosimilars guideline development – EGA’s perspective
Related content
FDA approves Poherdy (first interchangeable pertuzumab) and Armlupeg (pegfilgrastim) biosimilars
EMA recommends approval for insulin glargine biosimilar Ondibta and denosumab biosimilar Osqay
FDA approves denosumab biosimilars Osvyrti and Jubereq, Boncresa and Oziltus
FDA approves aflibercept biosimilar Eydenzelt and label expansion for adalimumab biosimilar Yuflyma
FDA approves Poherdy (first interchangeable pertuzumab) and Armlupeg (pegfilgrastim) biosimilars
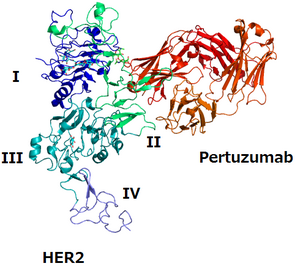
Biosimilars/News Posted 27/01/2026
EMA recommends approval for insulin glargine biosimilar Ondibta and denosumab biosimilar Osqay

Biosimilars/News Posted 16/01/2026
FDA approves denosumab biosimilars Osvyrti and Jubereq, Boncresa and Oziltus
Biosimilars/News Posted 07/01/2026
FDA approves aflibercept biosimilar Eydenzelt and label expansion for adalimumab biosimilar Yuflyma

Biosimilars/News Posted 05/12/2025
The best selling biotechnology drugs of 2008: the next biosimilars targets






Post your comment