Generics/Research
Impact of South Korea’s new drug–pricing policy on market competition
In April 2012, the Korean Government implemented a new policy to try and make its multiple sourced (off-patent) market more competitive. Their objective was to lower the price of generics through increased competition. The government in this way also aimed to reduce the costs for both patients [who have typically a 30% co-payment in ambulatory care (20% in hospitals)] and the National Health Insurance. The core of the policy was to establish the same maximum reimbursement price, i.e. the same ceiling price, for both the originator (brand-name) and the generic drug. This was expected to make the market more competitive, with generics manufacturers competing with each other to gain market share by lowering their prices. However, other professionals argued that this policy would still favour originators, given the general belief that an originator medicine, which is often from an international pharmaceutical company, would be better quality.
Is India ready to use only generics?
This editorial provides a balanced and neutral perspective of the debate regarding use of brand-name versus generic medicines, from an Indian endocrine point of view. It helps stakeholders arrive at appropriate decisions, using a process of informed and shared decision-making [1].
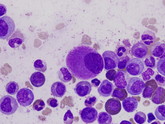
The satisfaction of healthcare payers, patients and physicians with generic imatinib
With the begining of the era of tyrosine kinase inhibitors (TKIs), chronic myeloid leukaemia (CML) became a chronic disease, in which good responding patients usually have a life expectancy similar to the age- and sex-matched normal population [1]. In many countries, the first-line treatment of chronic phase CML is imatinib mesylate (IM). Whereas, especially in some developed countries, second generation TKIs (dasatinib, nilotinib) which have deeper and faster responses, but are also more expensive than IM, are utilized in the upfront setting. The introduction of TKIs increased the prevalence of CML, and optimal responders to IM should continue therapy indefinitely, so the originator TKI treatment (Gleevec) surely put a strain on healthcare providers even in developed countries.
Competition in the generics industry
In theory, an increase in the use of generics should help to reduce overall drug expenditures. However, growth in spending on medicines in the US increased by US$46.2 billion, or 12.2%, over 2014 levels, reaching US$425 billion in 2015 [1]. This increase comes despite a simultaneous growth in spending on generics, which increased by US$7.9 billion (7.4%) to US$114.1 billion in 2015.
Generic antibiotics could be contributing to bacterial resistance
Therapeutic non-equivalence of generic antibiotics could be contributing to the global problem of bacterial resistance, according to researchers from the Universidad de Antioquia in Colombia.
Different approaches to bioequivalence trials for EMA evaluation
Selection of robust bioequivalence study designs is a difficult task for manufacturers of generics. Author Nathaniel Refalo from the Malta Medicines Authority and colleagues therefore investigated whether different approaches in various products assessed by the European Medicines Agency (EMA) during the approval phase resulted in a reduction in the resources required to show bioequivalence [1].
South Africa’s expedited registration policy not speeding up access to biosimilars
Since South Africa’s National Department of Health (DoH) implemented a fast-track registration policy in 2003 the large number of generics applications has led to a backlog in approvals [1]. This has led to concern that this backlog is having a detrimental effect on patient access to critical pharmaceutical medicines and in particular biosimilars [2].
South Africa’s expedited registration policy for rapid access to critical medicines under threat by generics
In 2003, the National Department of Health (DoH) of South Africa implemented a fast-track registration policy, not only for new chemical entities (NCEs) considered essential for national health and which may not be on the Essential Medicines List (EML) of South Africa, but also for all medicines on the EML, the majority of which are generics [1].
Driving down drug prices: how regulators can influence affordability
In recent years there has been increasing global concern over drug prices and their affordability. And what is the role played by regulators in drug pricing? This is the subject of discussion in a recent paper co-authored by the European Medicines Agency’s (EMA) Executive Director Guido Rasi, its Senior Medical Officer Hans-Georg Eichler, the Executive Director of Dutch Medicines Evaluation Board Hugo Hurts, and the President of the German Federal Institute for Drugs and Medical Devices Karl Broich [1]. Although the price of medicines is not within the regulatory remit, the authors find this an inescapable subject for debate and they outline possible regulatory interventions that could drive down drug prices.
Generics in seizure control
Are generic medicines for the control of epileptic seizures bioequivalent to their brand-name counterparts? Steven Karceski [1] has recently reviewed a study carried out by researchers at the Johns Hopkins University School of Medicine, Baltimore, MD, USA in which they determine the bioequivalence of generic seizure control medications [2].